In the last few months, Dr Jeannina Smith has seen organ transplant recipients who have been very careful throughout the pandemic venture out for one activity, contract Covid-19 and lose their transplant.
“I have been at the bedside of a transplant recipient” who “was very ill and in the hospital, and she got Covid the second time in a healthcare setting”, said Smith, medical director of the infectious disease program at University of Wisconsin Hospitals and Clinics. “She was sobbing because she said, ‘It’s so hard for me to see that people care so little about my life that wearing a mask is too much for them.’”
While much of US society has breathed a collective sigh of relief at no longer having to wear a mask in public, that freedom has placed people who are immunocompromised at risk, such as Smith’s patients. Nor are they the only ones. Older adults, the very young and those with long Covid are at greater risk too. So while for many Americans the pandemic increasingly feels over, for others – often the most vulnerable – it rages on.
As Smith puts it, “What troubles me as an infectious disease specialist with an interest in public health is the abandonment of the idea that public health exists to protect the most vulnerable.”
About 7 million people in the United States are immunocompromised, according to the American Medical Association. That includes people who are organ or stem cell transplant recipients, or who have cancer, certain genetic disorders or take an immunosuppressive medication.
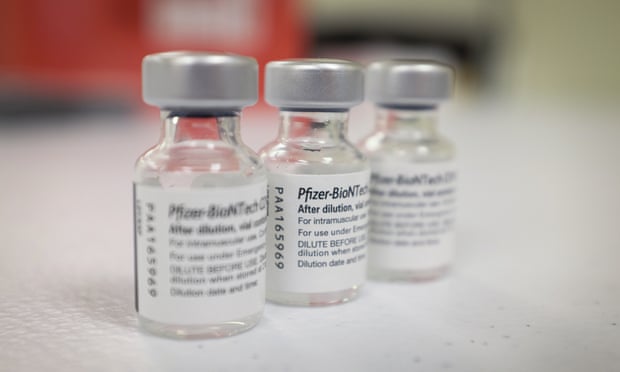
While there are now vaccines and better treatments for Covid and variants that appear to cause less severe disease than earlier ones, people like Smith’s patients still face a significant risk of becoming very sick or dying from Covid in part because they take medications that suppress their immune systems, she said.
“The problem is that the vaccination is less potent if you aren’t able to make a good immune response and so much of the protection that other people are afforded by vaccination” doesn’t protect transplant patients, Smith said.
And when the Centers for Disease Control and Prevention (CDC) stopped enforcing a mask mandate for public transportation in April, it made traveling harder for people who are immunocompromised, Smith said. Several of her patients contracted Covid while traveling.
“They have an increasing number of family members who are out and about, exposed and actually having Covid, and it makes them feel, rightly, that they are less able to do the things that they did safely,” Smith said.
Older adults also continue to face a greater risk from Covid. Of the more than 146,000 people who have died this year from Covid, 77% were over the age of 65.
“The risk of dying is not as great as it was before we had vaccines – not even close – but this is not a fun virus to get, and if you’re in your 80s, for example, you don’t really want to get any colds; you don’t want to get sick because you have less reserve,” said Dr Michael Wasserman, a geriatrician and chair of the Public Policy Committee of the California Association of Long Term Care Medicine.
But older adults must also balance that need for caution with the need for social engagement, which is also important to people’s health, Wasserman said.
That’s difficult in some senior housing where “the lazy approach to dealing with the health and wellness of older adults is to isolate them, and it takes away their choice”, said Wasserman. “We are at a point where this pandemic should not keep older people from socializing.”
The key for older adults is getting a second booster of the Covid vaccine, Wasserman said. He also recommends that older adults wear masks when they are indoors around people they don’t know.
“I don’t want to be alarmist. I think that’s the key here. I think people can live their lives,” he said. “I’m 63, and I’m doubly boosted, and when I go to the supermarket, I wear my N95” mask.
But wearing a mask can also be taxing on people who are required to do so in their jobs, said Erica Birkley, assistant professor of psychiatry and behavioral neuroscience in the University of Cincinnati College of Medicine.
“It can be a lot more difficult to get a sense of the other person’s emotions,” said Birkley, who also provides psychotherapy. “We also tend to drink less water or not take as many breaks throughout the day … We can get into a pattern of essentially being depleted in ways related to having to wear a mask.”
The key is ensuring that people can take mask breaks, she said.
It can also be helpful to think about how wearing a mask could benefit others, she said.
“It is usually going to be cathartic for me to think about the possible positive ripple effect for another human being in that room who possibly might be immunocompromised,” she said.
People with long Covid also often must contend with a lack of recognition of their disease, said Dr Monica Verduzco-Gutierrez, who chairs the department of physical medicine and rehabilitation at University of Texas Health Science Center at San Antonio and founded its Post-Covid Recovery Clinic.
Almost one in five US adults who had Covid continued to have long Covid symptoms in June, according to the National Center for Health Statistics.
Symptoms include severe fatigue; shortness of breath; heart palpitations; brain fog; and sleep problems.

“Even though yes, we are learning more, we don’t have a biomarker yet. We don’t have definitive treatments,” Gutierrez said. “A lot of people see it as a legitimate disease, and then I’m on social media … and occasionally people will say, ‘Well, how do you know it’s not just anxiety?’”
A new Brookings Institution report estimates that between 2 and 4 million people in the United States are out of work due to long Covid. Gutierrez said her patients can only obtain social security disability insurance or employer disability insurance benefits “very infrequently”.
“Everyone was hoping that they would get over it or that time will heal it, and they are just still not feeling that way,” Gutierrez said.
Before contracting Covid in January 2021, Jennifer Ramey spent almost three decades as a cardiology nurse and ran 20 marathons and hiked some of Colorado’s 14,000ft mountains.
“I loved what I did and was a hopeless romantic nurse and loved patient care,” she said.
But she has been out of work since February 2021 and feels exhausted after walking a couple of aisles at the grocery store, she said.
She spent eight months in rehab – some of it inpatient – working with physical, occupational, recreational and speech therapists. While she is now able to again drive, she still must do cognitive workbooks featuring pattern identification and word search exercises.
Ramey also lost her job.
She applied for disability benefits, but the Social Security Administration recently denied her. She plans to appeal. She does not expect that she will be able to return to work as a cardiology nurse.
“I should probably never check defibrillators and pacemakers. Even though I can do it in my head, I know my head is slower than it needs to be for something like that,” said Ramey. “I will never do the things that I loved as a nurse as far as the critical thinking part.”
Still, Gutierrez is encouraged by some of the recent research on long Covid. For example, a study from a Yale University researcher, which has not yet been peer-reviewed, found that cortisol levels were often lower among long Covid patients as compared to control groups.
That’s important because it could mean they are closer to identifying a biomarker for long Covid, which could lead to treatments and prove to “the naysayers, the insurance companies that this means you have long Covid, or this means you are impacted by long Covid”, Gutierrez said.
Smith, the transplant infectious disease specialist, also said she was hopeful that nasal vaccines under development could help reduce the risk of infection rather than just preventing severe outcomes, which would be helpful for her patients who are more vulnerable to the virus.
But even if that turns out to be the case, Smith remains discouraged by the lack of societal concern for such patients and doesn’t expect that to change.
“I think that the damage to public health is profound,” Smith said. “And in regards to Covid, I think likely permanent.”
Stay connected with us on social media platform for instant update click here to join our Twitter, & Facebook
We are now on Telegram. Click here to join our channel (@TechiUpdate) and stay updated with the latest Technology headlines.
For all the latest Covid-19 News Click Here
