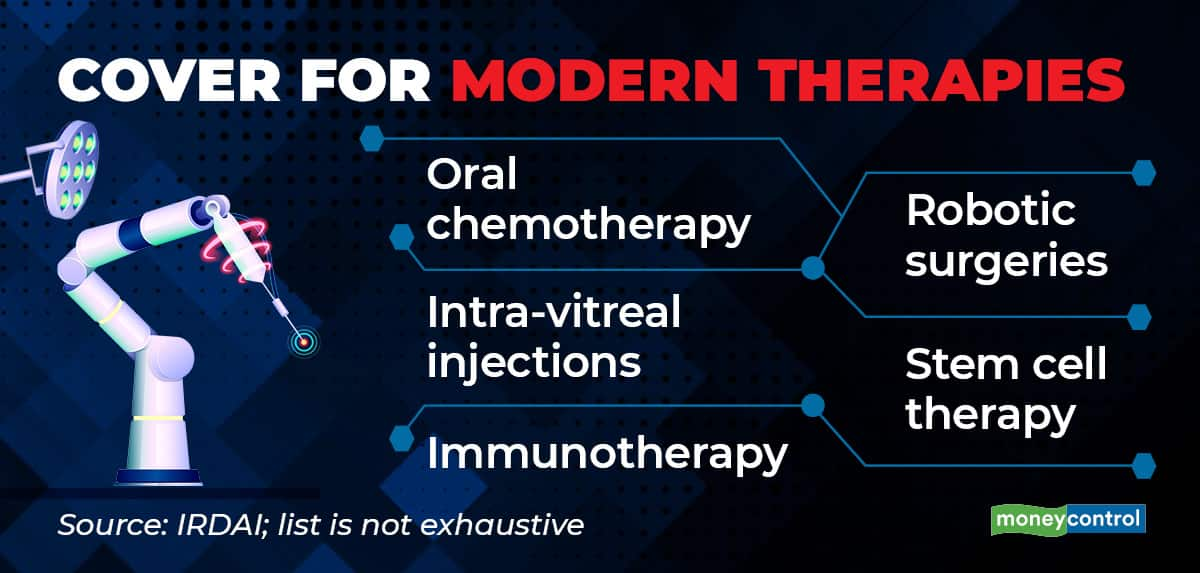
Recently, the insurance regulator IRDAI vetoed a few health insurers’ decision on a COVID-19 treatment. The insurance companies had termed monoclonal antibody cocktail treatment as experimental therapy and had rejected claims to cover it. The IRDAI did not allow this, saying that the therapy has been approved for emergency use in India. Usually, insurers do not pay for unproven or experimental therapies that are not based on “established” medical practices in India. That said, IRDAI’s standardisation of exclusion regulations framed in 2019 prohibit insurers from rejecting claims for modern treatment procedures, such as stem-cell therapy and robotic surgeries, though they can set sub-limits.
Stay connected with us on social media platform for instant update click here to join our Twitter, & Facebook
We are now on Telegram. Click here to join our channel (@TechiUpdate) and stay updated with the latest Technology headlines.
For all the latest World News Click Here